By: Sreejita Das
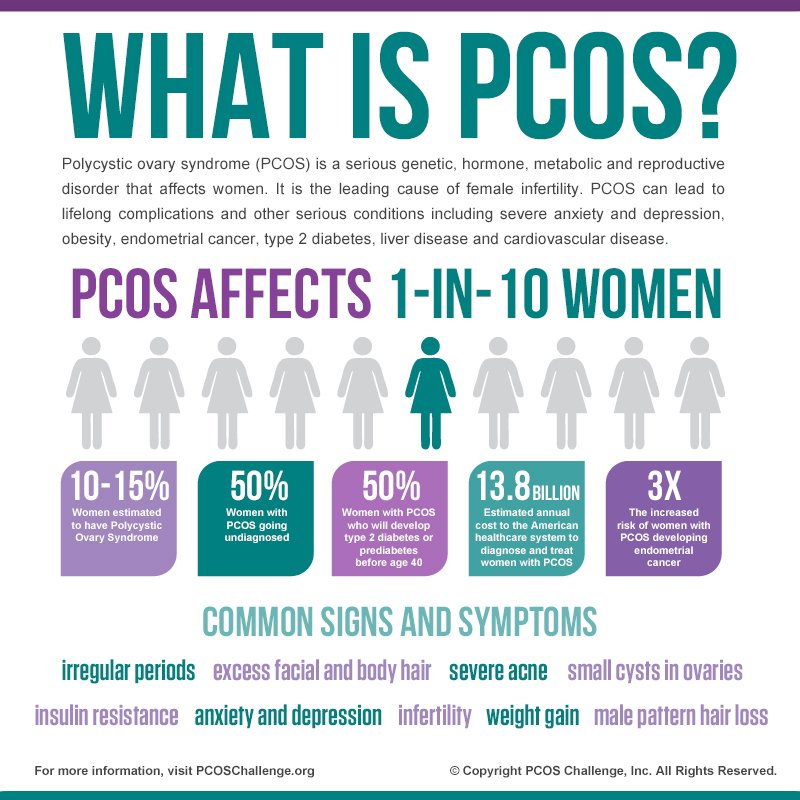
PCOS. It’s a common word I hear people say, especially when women are having issues with their menstrual cycle, but do people actually know about the condition? PCOS, otherwise known as Polycystic Ovarian Syndrome is a reproductive condition, where the ovaries produce a higher than normal amount of androgens (think sex-hormones typically seen in men. Think of the typical DHEA and testosterone).
On a physical level, these higher levels of androgens cause hirsutism (excessive and thicker hair growth on arm hair and facial hair) and hair loss. Another physical byproduct is the creation of an irregular menstrual cycle (missing cycles or consecutive cycles). Evidently, as the menstrual cycle is affected and unable to retain a normal hormone balance, fertility decreases.
On a molecular level, it affects metabolism as well. To elaborate, women with PCOS have difficulty either retaining weight or losing weight (majority of the women face this problem) causing issues with body image. This balancing act with metabolism is due to insulin resistance, making it difficult to stay within a healthy weight range. Furthermore, as the name polycystic ovarian applies, some women develop cysts in their ovaries, which can flare up and sometimes need to be surgically removed to prevent any further aching pain.
PCOS isn’t just a ‘missing periods issue’; it’s a syndrome that affects the daily lives of 1 in every 10 women. If you or anyone you know are facing similar symptoms, you should contact your doctor and request an ovarian ultrasound (to check for cysts), a blood test for glucose and androgens present or ask for a referral to a PCOS specialist! Even if you may not have PCOS, it could lead to a diagnosis of other reproductive health conditions (eg. endometriosis).
So how do people with PCOS deal with it? Simply put, we deal with it everyday. There is no simple cure or medicine we can take that makes it go away, but rather it’s a chronic condition. When women are diagnosed with PCOS, the options given to them are IUD insertions, birth control, medications (such as metformin to lower resistance or spironolactone to stop the metabolic pathway of testosterone) and a relatively restrictive diet with exercise (low carbs and low dairy products, a diet relatively hard to maintain over the long term).
As with every chronic condition, PCOS starts to affect you not only mentally, but physically as well; feeling tired and frustrated and that your body is ‘useless’ and unwilling to cooperate. It’s an uphill battle and a relationship that many struggle with. Fortunately, there’s various online communities that provide support to each other; these can be found on Reddit and Facebook, and are generally very supportive and willing to share their experiences with the condition.
Unfortunately, since PCOS is perceived as a ‘female’ issue, it has lacked research and funding, creating a cloud of mystery around it. However, as tides begin to shift, new studies and findings are beginning to emerge. I recently took part in a study that focused on the community aspect of the diagnosis phase and am super excited to see the results.
Another important factor to consider is that most women don’t get diagnosed. Sadly, the medical system is still very patriarchal and undermines the voices and experiences of women, while also being less informed about the female body, impeding on the ability for women to get proper diagnosis. If you ever suspect that you are being misdiagnosed or ignored, ask for a second opinion. September is PCOS month; it is a month to help raise awareness for this chronic condition and help support women who have PCOS, and destigmatize and demystify the condition. Aside from that, it also helps validate patients who are searching for a diagnosis.
If you’d like to learn more about the syndrome and events held during this month, check out https://pcosawarenessmonth.org!